
This post was prepared by Tiara Teders, PharmD Candidate, reviewed by Sean Reilly, BS Pharm, PharmD, RPh, BCOP.
September is National Prostate Cancer Awareness Month, which provides the perfect opportunity to heighten our understanding of this malignancy.
What is prostate cancer?
The prostate is a gland found only in males and is responsible for making a portion of seminal fluid. Anatomically, it is located below the bladder and anterior to (in front of) the rectum. In healthy males, the prostate is approximately the size of a walnut, but can increase in size with age. The most common type of prostate cancer is adenocarcinoma, a cancer that develops from the prostate gland cells responsible for the production of the prostate fluid that is added to the semen. Most prostate cancers are indolent (very slow growing), and therefore, may go unnoticed for an extended period.
How many men are impacted by prostate cancer?
Prostate cancer is one of the most common cancers in American men, only second to skin cancer. The American Cancer Society estimates that approximately 174,650 people will be diagnosed in 2019, and about 31,620 people will lose their life to prostate cancer.
Around 1 in 9 men will be diagnosed with prostate cancer during his lifetime. Fortunately, 95% of all prostate cancers are detected when the cancer is confined to the prostate, so treatment success rates are high, especially when compared to other cancers.
What is the prostate cancer survival rate?
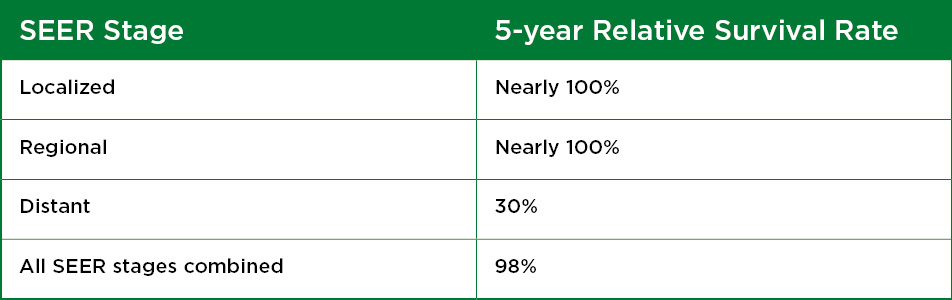
The National Cancer Institute maintains the SEER (Surveillance, Epidemiology, and End Results) database. SEER collects cancer incidence data from population-based cancer registries covering approximately 35% of the U.S. population. The SEER registries collect data on patient demographics, primary tumor site, tumor morphology, stage at diagnosis and first course of treatment, and they follow-up with patients for vital status. For prostate cancer, SEER tracks 5-year relative survival rates in the United States by grouping the cancer into localized, regional, and distant stages (rather than AJCC TNM stages).
- Localized – refers to disease that has not spread outside of the prostate (often AJCC stage I, II, and some III)
- Regional – denotes that the cancer has infiltrated nearby structures or lymph nodes (stage IIIB and IVA)
- Distant – means the cancer has spread to distant parts of the body (stage IVB)
Based on men diagnosed with prostate cancer between 2008 and 2014, 5-year relative survival rates are encouraging, as represented in the table below. These numbers apply to the stage of cancer when it was first diagnosed but does not consider recurrent or metastatic (spreading) disease.
Increased age is the biggest risk factor associated with the development of prostate cancer, however, it is not the only one. Other risk factors include:
- Genetic makeup increases prostate cancer risk and contributes to about 40% of all prostate cancers. Prostate cancer tends run in families, so men with a close relative with prostate cancer may be twice as likely to develop the disease.
- African American men are 76% more likely to develop prostate cancer compared to white men, and 2.2 times more likely to die from the disease.
- Social and environmental factors such as a high-fat, high-processed-carbohydrate diet or being overweight/obese put men at an increased risk of disease development.
When should men be screened for prostate cancer?
Because early stages of prostate cancer are asymptomatic, there aren’t any early warning signs. Screening at-risk patients is the best means of early identification.
There is some controversy surrounding the risks and benefits of prostate cancer screening. Screening is generally recommended based on individual risk. In healthy men with no unusual prostate-related symptoms, screening should begin based on the following parameters:
- Age 40 for men with a family history of prostate cancer
- Age 45 for African American men
- Age 50 in men with no family history of prostate cancer (and are not African American)
- Men between the ages of 55 and 69 should discuss screening with their provider
- Screening is not recommended in men over 70 years of age
Screening methods
There are two primary methods of prostate cancer screening: DRE and PSA.
A Digital Rectal Exam (DRE) is a physical exam in which a qualified health care provider inserts a finger into the rectum in order to feel the back wall of the prostate gland for abnormalities (enlargement, tenderness, lumps, or hard spots).
The Prostate Specific Antigen (PSA) test measures the level of PSA in a man’s blood. PSA is a protein produced by the prostate and is normally found in the semen, with small amounts released in the bloodstream. In addition to prostate cancer, a few benign (not cancerous) conditions can cause a man’s blood PSA level to rise. The most frequent benign prostate conditions that cause an elevation in PSA level are prostatitis (inflammation of the prostate) and benign prostatic hyperplasia (BPH) (enlargement of the prostate). There is no evidence that prostatitis or BPH leads to prostate cancer, but it is possible for a man to have one or both conditions and to develop prostate cancer as well.
When PSA becomes highly elevated, it can be easily detected with this blood test. PSA levels do not diagnose prostate cancer and may not even be present in all patients with prostate cancer. It is important to know that several factors can influence PSA levels, such as age, prostate size, prostatitis, benign prostatic hyperplasia, urinary tract infection or irritation, prostate stimulation and medications (finasteride, dutasteride).



