
This post was written by Amber Glessner, NP, Parkview Vein Clinic.
There are many methods available to help prevent pregnancy. Deciding which option is right for you requires the consideration of several factors, including potential side effects, convenience, cost and your future pregnancy plans. When it comes to the common use of birth control with hormones, patients often have questions about any potential risks, including the development of blood clots. In this post, we’ll go over how these products work and what women need to know before they make a decision.
What’s in hormonal birth control?
Hormonal methods of birth control are a safe and reliable approach to contraception for most women, and come in the form of pills, implants, intrauterine devices (IUD), injections, vaginal rings and contraceptive skin patches.
These methods contain synthetic hormones—a combination of estrogen and progestin, or just progestin. Some varieties of pills, contraceptive patches and vaginal rings have both hormones. Pills that contain both estrogen and progestin are referred to as “combination pills,” while the progestin-only pills are called “pop” or the “minipill.”
In the 1970s and ‘80s, birth control pills typically contained 50 micrograms of estrogen. Today, the highest amount in a birth control pill is around 35 micrograms, and some options have as little as 20 micrograms.
Does all contraception include hormones?
No. Nonhormonal methods include the copper IUD, barrier methods (such as condoms), the cervical cap, diaphragm and sponge.
What makes blood clots so dangerous?
We have two sets of veins–deep and superficial. Deep vein thrombosis (DVT) is a condition that occurs when a blood clot (thrombus), also known as venous thromboembolism (VTE), develops in the veins deep in the body. The blood clot may partially or completely block blood flow through the vein.
Most DVTs occur farther away from the heart, happening in the lower leg, thigh or pelvis, but they can also occur in other parts of the body, including the arm, brain and other organs. If the DVT travels to your lungs, it’s called a pulmonary embolism (PE). According to Cleveland Clinic,
“Each year, approximately 1 to 3 in every 1,000 adults develop a DVT or pulmonary embolism in the United States, and up to 300,000 people die each year as a result of DVT/PE. It’s the third most common vascular disease, behind heart attacks and strokes. Acute DVT/PE can occur at any age but are less common in children and adolescents and more common in those over the age of 60.”
How much does estrogen increase the risk for developing a blood clot?
The liver makes dozens of pro-clotting and anti-clotting factors. While the exact reason is unknown, estrogen influences the way the liver makes those pro-clotting factors. Though there are numerous factors involved in the clotting process.
Here is what we can extract from the current data:
- The risk of venous thromboembolism (VTE) has a three to five-fold increased relative risk in combined oral contraceptive (COC) pill users.
- Hormonal birth control that contains estrogen more commonly contributes to an increased risk of blood clots.
- The pill and the ring appear to have similar risks for estrogen-containing birth control.
- Researchers have found mixed data about the patch—namely, that it might present a higher risk of blood clots as compared to pills or rings.
- In contrast, progestin-only products are not associated with an increased risk of VTE.
- The increased risk for a birth control-related blood clot is small. At most, 10 in 10,000 people per year develop these clots as a result of being on birth control, and only hormonal birth control that contains estrogen increases your risk.
- Combined hormonal contraception options are associated with an increased relative risk of thrombotic events, however, the absolute risk remains low in most healthy, nonsmoking women.
In fact, you’re more likely to develop a blood clot from pregnancy than you are from hormonal birth control. Blood clots are not very common in people of reproductive age. If you aren’t on any contraception or pregnant, the chance of developing a VTE is somewhere between one and five per 10,000 people per year.
The FDA’s research Source found that:
- Out of every 10,000 women taking birth control pills, three to nine of them will develop a blood clot.
- Out of every 10,000 women who are not pregnant and who do not use birth control pills, one to five of them will develop a blood clot.
- Out of every 10,000 pregnant women, five to 20 of them will develop a blood clot.
- Out of every 10,000 women in the first 12 weeks after giving birth, 40 to 65 of them will develop a blood clot.
Figure 1: Likelihood of Developing a Blood Clot
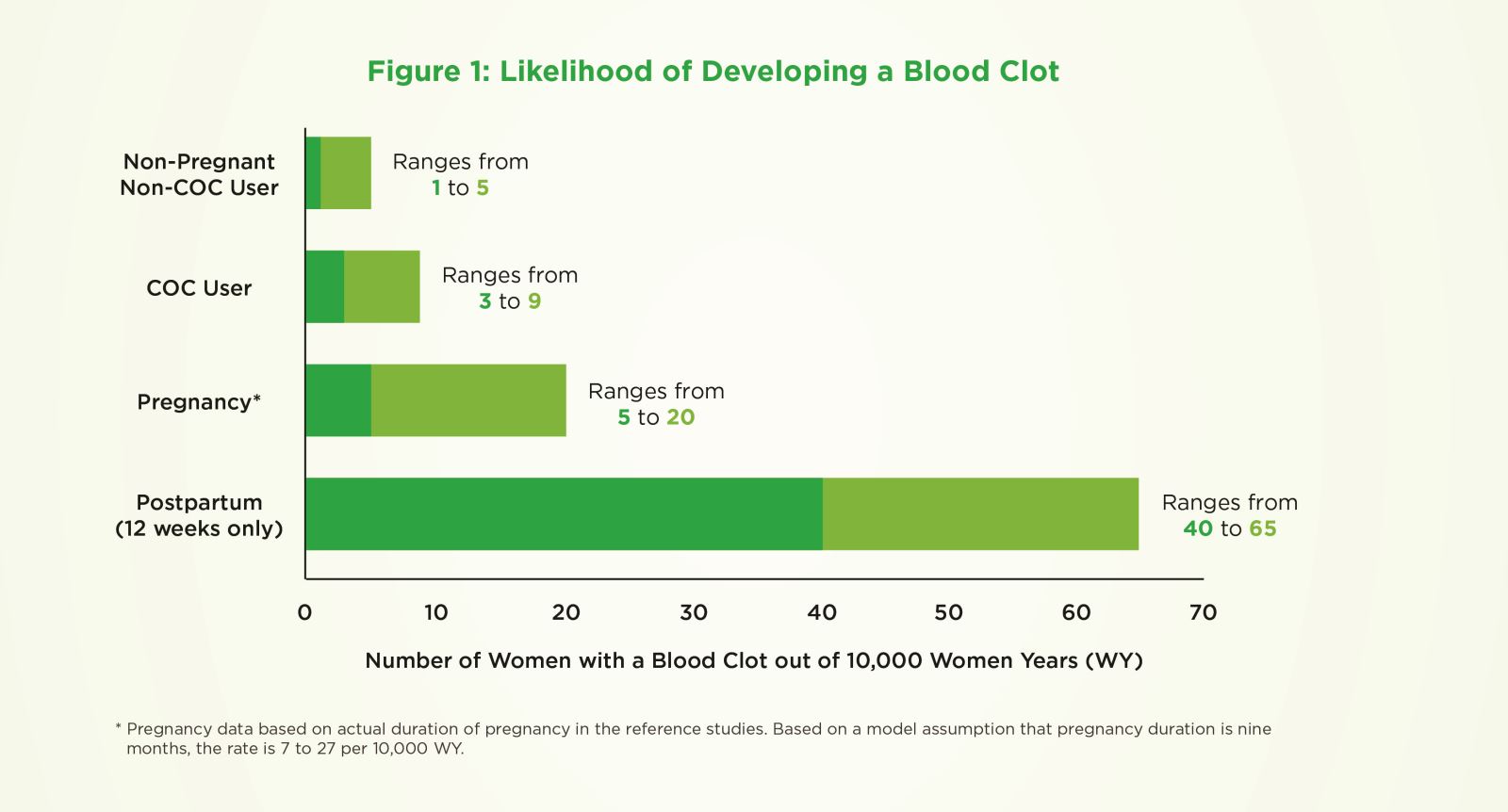
COC = combination oral contraceptives or birth control pills
Why does pregnancy increase your blood clot risk?
Pregnancy increases your risk of developing blood clots because of hormonal and body changes that happen throughout the process. This heightened association with VTE may be due in part to obstruction of venous return by the enlarged uterus, as well as the hypercoagulable state associated with pregnancy. Estimates of the age-adjusted incidence of VTE range from five to 50 times higher in pregnant versus non-pregnant women.
This risk doesn’t end once you give birth, though. In fact, the increased blood clot risk stays high even in the postpartum period. Pregnancy-related hematologic changes return to baseline by six to 12 weeks after delivery. The prothrombotic state takes weeks to resolve, so postpartum individuals remain at an increased risk for thromboembolic disease for some time beyond giving birth.
Blood clot signs you shouldn’t ignore – recognizing the symptoms of DVT
Symptoms can vary, but common signs of DVT include:
- Swelling of the leg or arm (sometimes suddenly), warmness to the area with red or discolored appearance.
- Pain or tenderness in the leg or arm (may only happen when standing or walking).
- The veins near the skin’s surface might appear larger than normal.
- Abdominal or back pain (when blood clots affect the veins deep inside your abdomen).
- Severe headache and/or seizures (when blood clots affect the veins of your brain).
- Symptoms progress instead of improving.
Some people don’t know they have a DVT until the clot moves from their leg or arm and travels to their lung. When the clot is in the lungs, it’s called a pulmonary embolism (PE). Symptoms of PE include:
- Chest pain
- Shortness of breath
- Lightheadedness
- Blood when coughing
- Fainting
Prevention
There are some ways you can reduce your risk of developing blood clots, such as:
- Avoid prolonged periods of standing or sitting in one spot. Exercise your calf muscles if you need to sit still for a long time. Stand up and walk at least every hour if you’re on a long flight or get out of the car every hour if you’re on a long road trip.
- Avoid staying in bed for long periods of time. Get up and move around as soon as you can after you’re sick or have surgery. The sooner you move around, the less likely you are to develop a DVT.
- Take medications as prescribed and use compression stockings after surgery (if your provider prescribes them) to reduce your risk of a blood clot. Some surgeons will place patients on blood thinners after surgery to prevent clots from forming.
- If you have varicose veins, monitor your symptoms and talk with your doctor about having them evaluated. Wearing compression stockings can help promote upward blood flow and prevent the pooling of blood in the veins. If you’ve had previous clotting events, wearing knee-high compression stockings can minimize leg pain and swelling.
- Avoid activities that may cause a serious injury (e.g. leg-crushing injuries from heavy equipment, motor vehicle accidents, falls/fractures).
- Stay hydrated at all times, and especially during travel.
But some risk factors for blood clots, are out of your control, including:
- Family history
- Age (40+)
The role of comorbidities in blood clot risk
The World Health Organization (WHO) estimates that the global prevalence of obesity nearly tripled between 1975 and 2016, with 15% of adult women falling into the category. The risk of VTE increases as body mass index (BMI) rises, and doubles for women considered obese, versus those who are not. Obesity has the most substantial impact on VTE in women under 40 years of age, who have a five-fold increased risk compared with non-obese women.
It’s important to talk to your provider about your medical history and diagnoses before making any decisions about hormonal contraception. If you have a history of blood clots, a genetic factor that increases your risk of blood clots or thrombophilias (a word used to describe underlying conditions that cause blood clots), hormonal birth control might not be the right option or you. Additionally, those living with high blood pressure or migraine with aura also have an increased risk of strokes and heart attacks, so it would be best to consult with your doctor before beginning a hormonal contraceptive.
More information
The Centers for Disease Control and Prevention (CDC) app US MEC US SPR offers recommendations for contraceptive methods, categorized by gender and existing medical conditions, as well as other criteria. This information is intended to assist healthcare providers when they counsel women, men and couples about contraceptive method choice, but is a helpful tool for patients as well.
Don’t hesitate to talk to your doctor about your questions and concerns. They can help you arrive at a birth control method you feel comfortable with.




