This post was written by Caylie Cappelli, NP, Integrative Medicine.
Our autonomic nervous system functions instinctively; we don't have to think about it, and we have no conscious control over it. It regulates processes such as heart rate, digestion, blood pressure and sweating. Postural Orthostatic Tachycardia Syndrome (POTS) is a dysregulation of these automatic processes. Most notably, it causes a significant increase in heart rate upon standing, often accompanied by other symptoms. This differs from the brief lightheadedness some people feel after standing up quickly, which typically resolves on its own.
In this post, we'll go over how this condition presents, why it might happen and ways to make living with it more manageable.
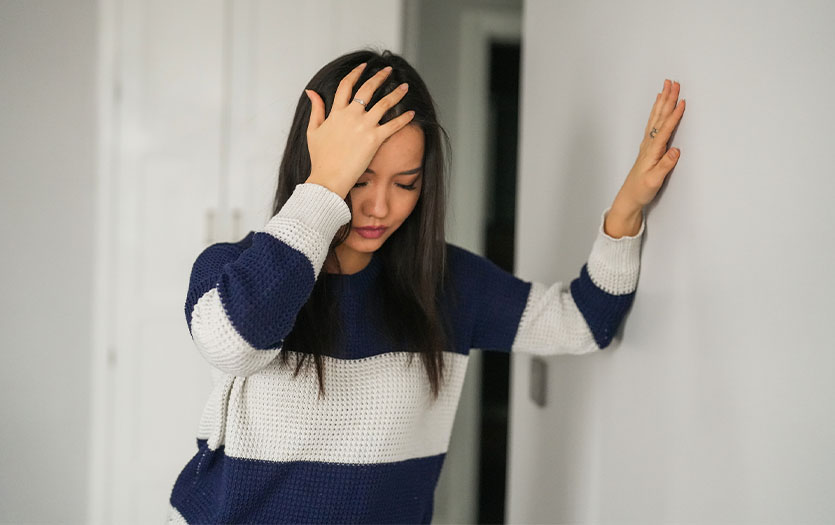
Symptoms
Symptoms of POTS can be vague and difficult to articulate. Many patients simply report that they "don't feel good," and it can take years to reach a diagnosis. However, since COVID-19, awareness has grown due to the increase in POTS-like symptoms post-infection.
Common symptoms include:
-
Shortness of breath (especially noticeable when climbing stairs)
-
Heart palpitations (a fluttering feeling in the chest)
-
Elevated heart rate upon standing
-
Dizziness or lightheadedness
-
Feeling faint or near-syncope
-
Brain fog
Symptoms often worsen in the morning, especially when transitioning from lying to sitting or standing, and can last for hours or even all day. Most patients feel better when lying down.
Causes
Several factors can cause POTS, though many cases remain idiopathic (no known cause). It affects both children and adults and is particularly common in females during puberty due to hormonal changes, though some may outgrow it. Other potential triggers include:
Even with these associations, many patients are unable to pinpoint a definitive cause.
Testing
A common in-office screening is orthostatic vital sign testing, in which the patient's heart rate and blood pressure are recorded in the lying, sitting and standing positions.
-
A positive result typically shows an increase of 30 beats per minute or more upon standing, prompting referral to cardiology.
-
A negative result does not rule out POTS. Further testing may be required depending on the symptoms observed.
Further diagnostic tests can include:
-
Echocardiogram (ultrasound of the heart)
-
Electrocardiogram (EKG) to evaluate heart rhythm
-
Holter monitor worn for 24–48 hours (or longer)
-
Tilt table testing
Treatment
There is no universal treatment for POTS; condition management typically focuses on supporting lifestyle changes and, in some cases, cardiac medications prescribed by a primary care provider or cardiologist.
At Parkview Physicians Group – Integrative Medicine, we help patients build habits in four key areas:
-
Nutrition
-
Sleep
-
Stress management
-
Exercise
These changes can be challenging, but we work with patients to introduce them gradually. Tips and strategies include:
-
Sleep: Quality rest can dramatically impact daily symptoms.
-
Nutrition: Eating small, frequent meals of whole foods can help. Avoid heavily processed or high-carb foods, which may worsen symptoms.
-
Hydration: Drink 8–16 ounces of water before getting out of bed.
-
Salt intake: Increased sodium helps raise blood pressure and reduce heart rate. Can use electrolyte drinks or consider salt tablets under guidance.
-
Compression garments: Not fashionable, but effective. Knee-high and thigh-high compression stockings help improve circulation. Bike shorts may also help by applying gentle abdominal pressure.
-
Avoid hot showers or baths: Heat can exacerbate symptoms by dilating blood vessels, which can raise heart rate.
-
Exercise: Though it may seem counterintuitive, regular movement is crucial. Deconditioning worsens symptoms. Start slowly—seated exercises or short walks—and build endurance gradually.
Outlook
POTS symptoms can be distressing and often mimic more serious conditions, but it is a manageable disorder. Improvement takes time and experimentation, and each patient’s journey is different. We encourage patients to:
-
Listen to their body
-
Take breaks and rest when needed
-
Eat well and stay hydrated
-
Move regularly
-
Reduce stress when possible
Integrative Medicine can support patients in making these changes and improving overall wellness. For more information or to schedule an appointment with an Integrative Medicine provider, please call our office at 260-672-6590.